Psoriasis
Hello everyone, thank you for all the amazing support we are so grateful. On week 233 we are sharing a compelling post, so many people are affected with Psoriasis and I have personally witnessed people that fully overcame it. So here we have authorities on the matter contributing valuable information for you to share or use yourself if you happened to be affected by this condition. In the years that I have worked with skin, I experienced first-hand the physical and mental consciousness on people, the shame and self-confidence, the isolation and even depression from having to endure the facts and side effects of Psoriasis. We are determined to share research and tips with well-founded facts to make a difference in anyone’s life that is affected. if you know someone that is afflicted with this condition please share the information, it is devastating for the ones that do.
Thank you from all of us at Isabel’s Beauty Blog
Psoriasis is a chronic disease of your immune system that causes cells to build up on the surface of your skin, leading to thick, red, scaly patches that are very itchy and sometimes painful. Up to 7.5 million Americans suffer from this condition, which has a surprisingly significant economic impact as well.
A new study in JAMA Dermatology reported that direct US healthcare costs related to psoriasis treatment may be up to $63 billion a year. There were also indirect costs (such as loss of work hours) of up to $35 billion and another $35 billion in costs related to associated health problems, like heart disease and depression.
Taken together, the researchers found the annual US cost of psoriasis amounted to approximately $112 billion in 2013.
Psoriasis Is More Than a Superficial Skin Condition

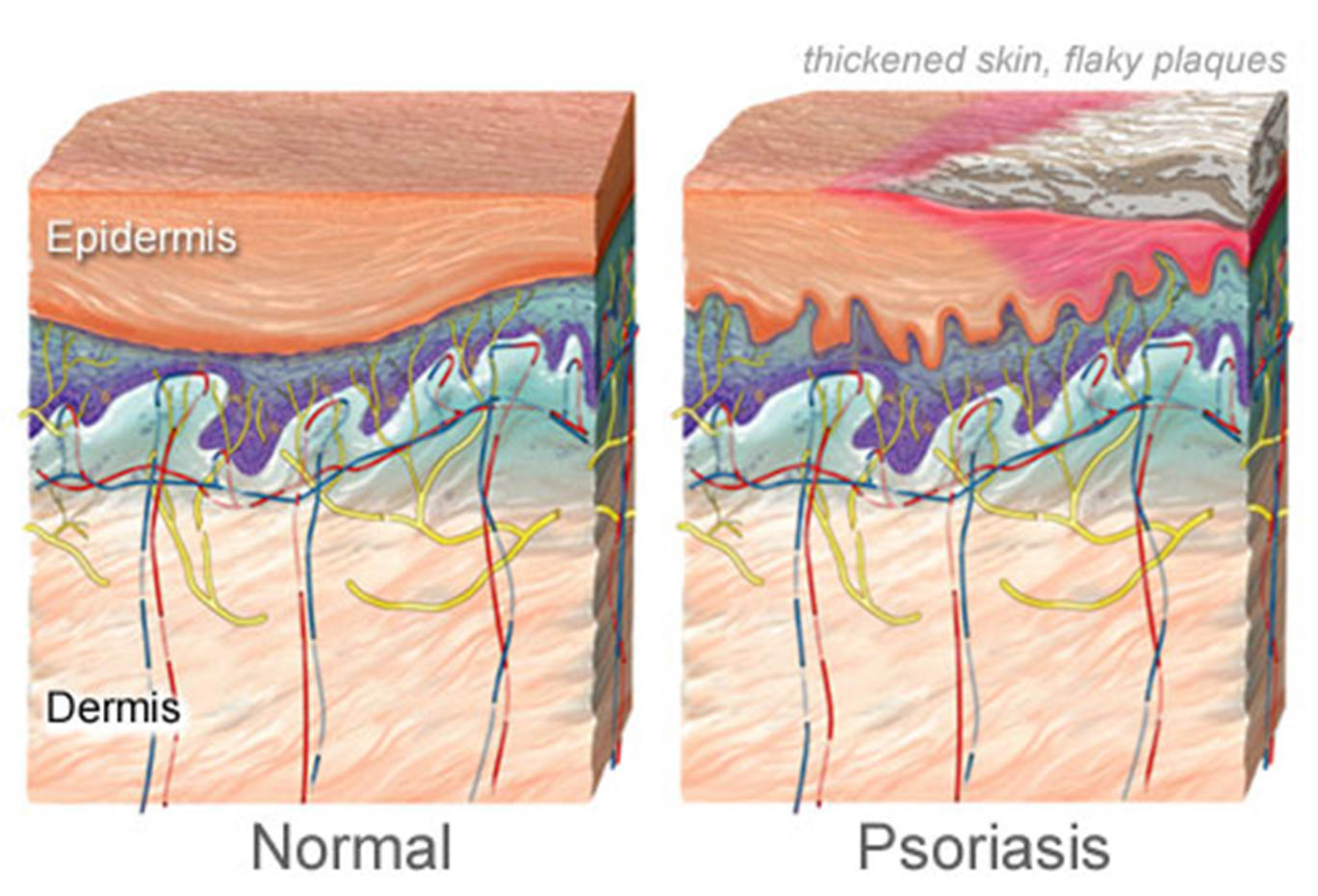
Although psoriasis appears as a skin condition, it is actually an autoimmune disease. Part of the reaction occurs when a type of white blood cell called a T cell mistakenly attacks healthy skin cells.
These overactive T cells then proceed to trigger other immune responses that collectively speed up the over growth cycle of skin cells, causing them to move to the outermost layer of your skin in a matter of days rather than weeks.
Because the dead skin cannot be removed quickly enough, it builds up into really thick patches characteristic of psoriasis. For up to 60 percent of people with psoriasis, the condition seriously impacts their daily life and their confidence.
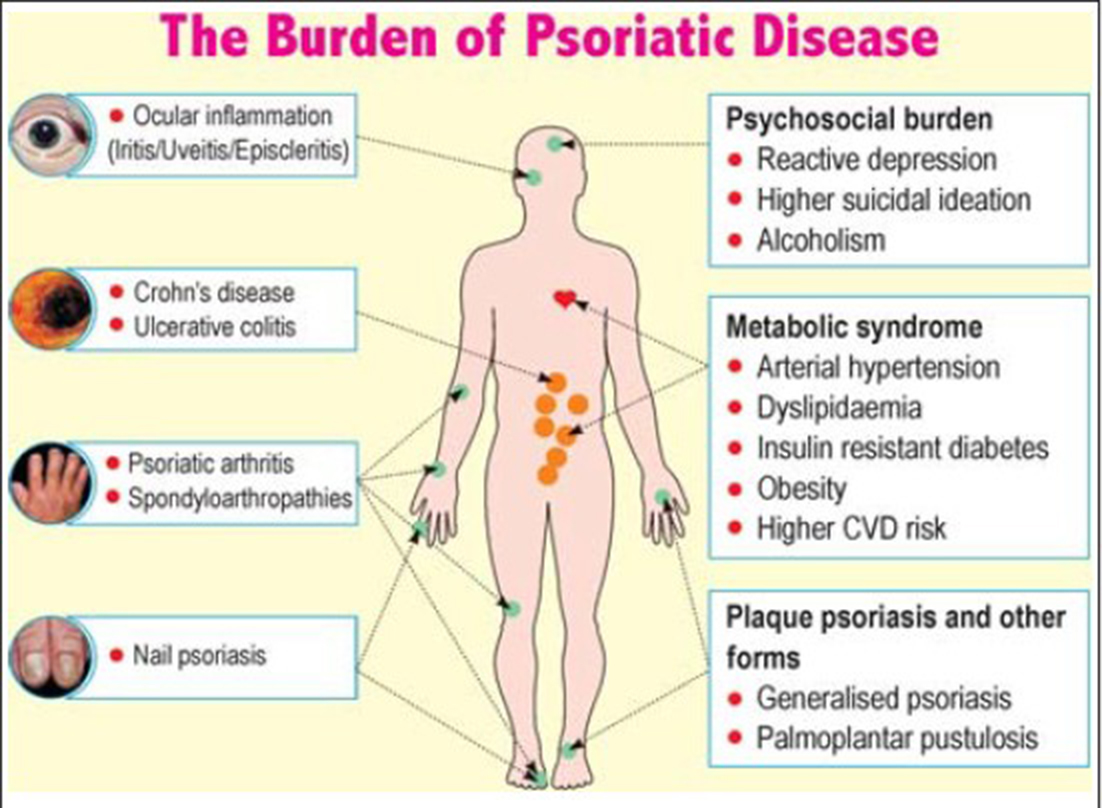
The skin may become so inflamed that it cracks and bleeds. Up to 30 percent of sufferers also develop psoriatic arthritis, which can cause debilitating joint damage.
People with psoriasis are also at an increased risk of numerous other chronic diseases, including eye conditions, type 2 diabetes, high blood pressure and heart disease. And then there are the psychological repercussions.
Those who aren’t familiar with psoriasis may view it as a contagious rash, and as a result people with psoriasis may be shunned or excluded socially,becoming reclusive. People with psoriasis often suffer from depression, low self-esteem, social isolation and problems at work, which may lead to a lower income.
Vitamin D Is Crucial for Autoimmune Diseases, Including Psoriasis
If you have psoriasis, it is imperative that you have your vitamin D levels tested and maintain levels in the therapeutic range of 50-70 ng/ml year-round. Vitamin D is a potent immune modulator, making it very important for the prevention of autoimmune diseases.
Great Vitamin D test kit Dr Mercola: http://shop.mercola.com/product/vitamin-d-testing-kit,1090,438,0.htm

According to one study, “vitamin D could have important immunomodulatory effects in psoriasis,” but unfortunately 80 percent of patients in winter, and 50 percent in the summer, were vitamin-D deficient.
Vitamin D is thought to affect psoriasis on multiple levels, including helping to regulate keratinocyte (skin cell) growth and differentiation as well as influence the immune functions of T lymphocytes and other cells. Vitamin D also inhibits cytotoxic T cells and natural killer cell activity, potentially helping to regulate skin cell growth.
In fact, not only are vitamin D derivatives commonly used as a topical treatment for psoriasis, but phototherapy is also a preferred type of treatment.
There is also at least one published report of a specific type of drug-induced psoriasis resolving after high doses of vitamin D3 were given to treat vitamin-D deficiency.
Existing psoriasis drug treatments are risky and expensive. NPR followed one man with psoriasis who has taken multiple prescription drugs for psoriasis, including experimental drugs and is still suffering.
One of the drugs, Raptiva, was pulled from the market for increasing the risk of deadly brain infections. Another Stelara, worked, but only for five years when his symptoms returned. In those five years alone, he reported the drug costs added up to $250,000.So is best to do a full research before creating more and bigger problems.
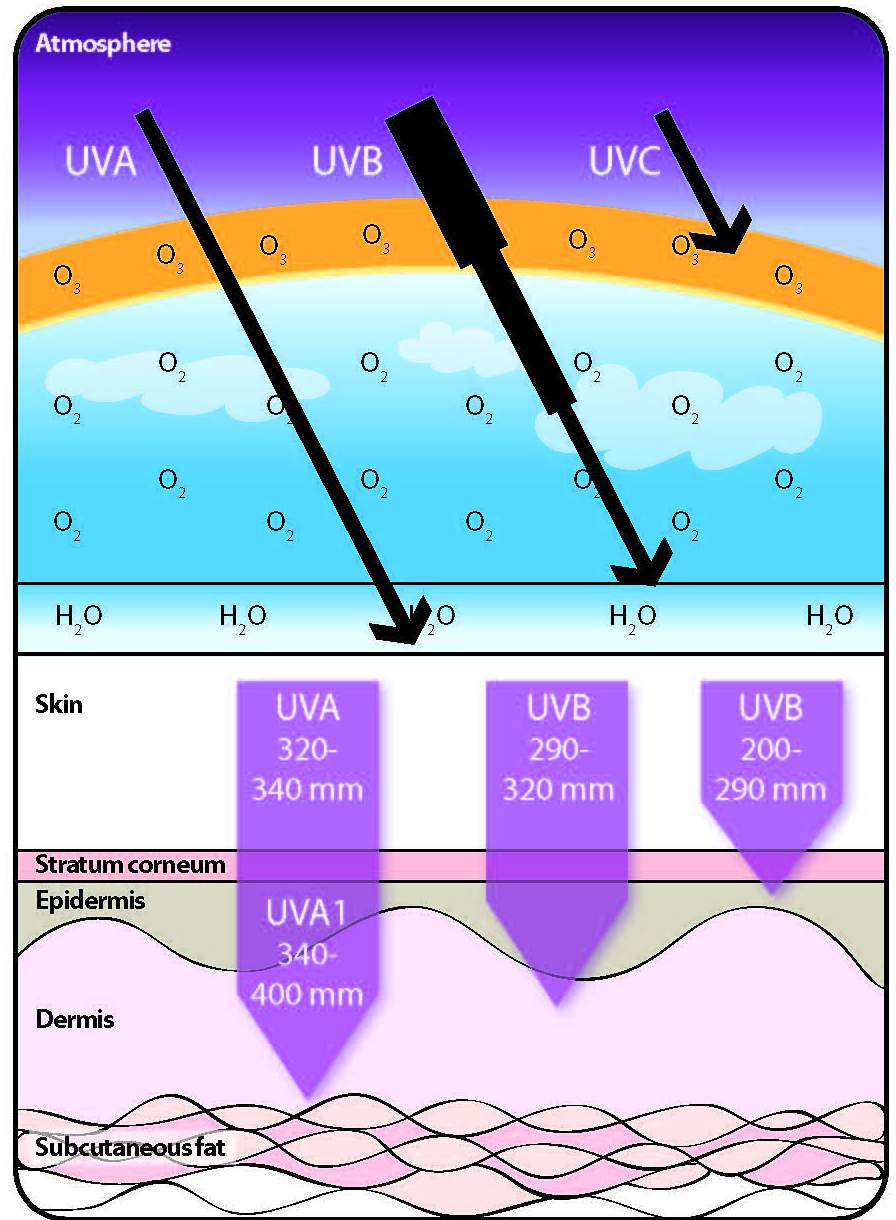
One of the most common psoriasis treatments is the drug psoralen combined with UV light exposure (known as PUVA). Psoralen makes your skin more sensitive to UV light, but it is often combined with UVA exposure. UVA rays are the type associated with skin damage, while UVB light causes your skin to produce vitamin D.
Optimize Your Vitamin D Levels If You Have Psoriasis
Typically, the best psoriasis treatment is exposure to sunlight to optimize your vitamin D levels. You don’t need to visit a dermatologist; you can do it yourself.
Speaking out in a professional capacity against this idea can cost you. In 2004, Dr. Michael Holick published the book, The UV Advantage, in which he encouraged readers to get some sensible sun exposure.
Ultraviolet Light from by Philips

At the time, he was a professor of dermatology because of the work he’d been doing with active vitamin D for the treatment of psoriasis. In fact, he’d received the American Skin Association’s Psoriasis Research Achievement Award—a rather prestigious award.
“As a result, I was in the department of dermatology, continuing to do psoriasis research. But once I began recommending sensible sun exposure for vitamin D, which is counter to what the American Academy of Dermatology’s message was, I was asked to step down as professor of dermatology back in 2004…
The American Academy of Dermatology still recommends: you should never be exposed to one direct ray of sunlight for your entire life.”
This is highly counterintuitive, given the research showing how beneficial vitamin D is for psoriasis. Sunlight exposure works, in part, because UV rays in sunlight and certain types of artificial light kill off the activated T cells in your skin.
This slows down cell turnover and reduces the scaling and inflammation of your skin.
Proper sunlight exposure will help you get your vitamin D levels into the therapeutic range, which has additional health benefits as well. It’s probably no coincidence that people with psoriasis, who are often vitamin D deficient, have an increased risk of chronic diseases like heart disease and metabolic syndrome – which are also associated with low vitamin D.
Have You Checked Your Vitamin D Level Lately?
While the optimal level for general health lies between 50-70 ng/ml, when treating chronic diseases such as cancer, heart disease, and autoimmune (i.e. psoriasis) and/or neurological diseases, your level should ideally be somewhere between 70-100 ng/ml, which is about double what is typically considered “normal.”
It’s important to realize that vitamin D deficiency is common around the world, even in areas where you’d suspect most people would get plenty of sun exposure. One recent study done in India found that 69 percent of 37,000 people tested across the country were vitamin D deficient (at or below 20 ng/ml), and another 15 percent had insufficient levels (20-30 ng/ml). Men between the ages of 31-60 and women aged 16-30, were at highest risk of vitamin D deficiency, although in the US the elderly are also seriously at risk.
The ideal method to optimize your vitamin D levels is through sensible UVB exposure. You can also use an oral supplement of vitamin D3. GrassrootsHealth has a helpful chart showing the average adult dose required to reach healthy vitamin D levels based upon your measured starting point. Many experts agree that 35 IUs of vitamin D per pound of body weight could be used as an estimate for your ideal dose, but you’ll need to test and monitor your levels to be sure.
If Taking a Vitamin D Supplement, Remember K2 and Magnesium, Too
If you opt for a supplement, be sure to take vitamin D3—not synthetic D2—and take vitamin K2 and magnesium in conjunction with it. Vitamin D is fat-soluble, so taking some form of healthy fat with it will also help optimize absorption. The biological role of vitamin K2 is to help move calcium into the proper areas in your body, and without sufficient amounts, calcium may build up in areas such as your arteries and soft tissues. This can cause calcification that can lead to hardening of your arteries—a side effect previously thought to be caused by vitamin D toxicity. We now know that inappropriate calcification is actually due more to lack of K2 than simply too much vitamin D.
Magnesium is also important, both for the proper function of calcium and for the activity of vitamin D as it converts vitamin D into its active form. Magnesium also activates enzyme activity that helps your body use the vitamin D. In fact, all enzymes that metabolize vitamin D require magnesium to work. As with vitamin D and K2, magnesium deficiency is also common, and if you’re lacking in magnesium and take supplemental calcium, you may exacerbate the situation.
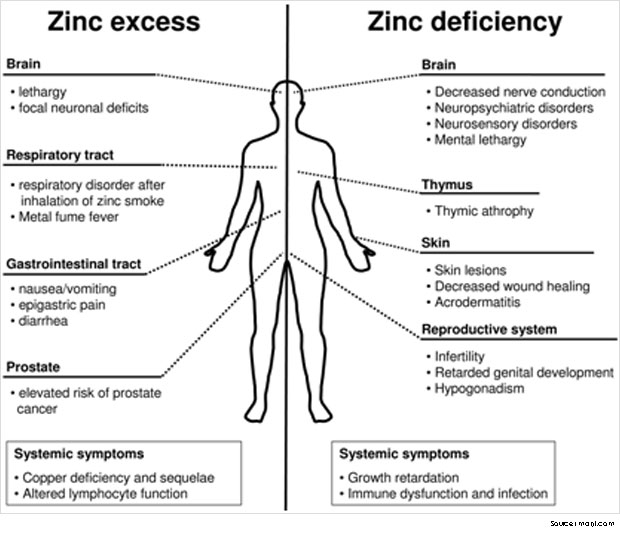
Vitamin A, zinc, and boron are other important cofactors that interact with vitamin D. When taking supplements, it can be easy to create lopsided ratios, so getting these nutrients from an organic whole food diet and sensible sun exposure is generally your best bet. Dietary sources of magnesium include sea vegetables, such as kelp, dulse, and nori. Vegetables can also be a good source. As for supplements, magnesium citrate and magnesium threonate are among the best.

How Vitamin D Performance Testing Can Help Optimize Your Health
A robust and growing body of research clearly shows that vitamin D is absolutely critical for good health and disease prevention. Vitamin D affects your DNA through vitamin D receptors (VDRs), which bind to specific locations of the human genome. Is it any wonder then that no matter what disease or condition is investigated, vitamin D appears to play a crucial role? This is why I am so excited about the D*Action Project by GrassrootsHealth. It is showing how you can take action today on known science with a consensus of experts without waiting for institutional lethargy.
It has shown how by combining the science of measurement (of vitamin D levels) with the personal choice of taking action and, the value of education about individual measures that one can truly be in charge of their own health. In order to spread this health movement to more communities, the project needs your involvement. To participate, simply purchase the D*Action Measurement Kit and follow the registration instructions included. (Please note that 100 percent of the proceeds from the kits go to fund the research project. I do not charge a single dime as a distributor of the test kits.)
As a participant, you agree to test your vitamin D levels twice a year during a five-year study and share your health status to demonstrate the public health impact of this nutrient. There is a $65 fee every six months for your sponsorship of this research project, which includes a test kit to be used at home, and electronic reports on your ongoing progress. You will get a follow-up email every six months reminding you “it’s time for your next test and health survey.”
Both eczema and psoriasis are potentially allergic conditions that can be triggered by environmental factors and dozens of other external irritants like:
-
Laundry detergent
-
Soaps
-
Household chemicals
-
Workplace chemicals
-
Perfumes
-
Animal dander
-
Metals (such as nickel in jewelry)
While psoriasis is most often linked with external allergic triggers, eczema is often caused by food allergies.
However, although they’re different diseases and have varying triggers, their treatments have many commonalities.
How to Effectively and Inexpensively Treat Eczema and Psoriasis

Eczema is “the itch that rashes,” meaning, there’s really no rash until you start scratching the itchy area. Hence, the first thing you need to do is to stop scratching!
Addressing the itch — As anyone with eczema will attest, this is easier said than done. But fortunately, there IS a really simple, inexpensive way to relieve the itch: Simply put a saltwater compress over the itchy area.
You’ll want to use a high-quality natural salt, such as Himalayan salt. Simply make a solution with warm water, soak a compress, and apply the compress over the affected area. You’ll be amazed to find that the itching will virtually disappear!

Another method that can be helpful for reducing or stopping the itch is EFT.
Proper skin hydration – When working with any type of skin condition, you need to make sure your skin is optimally hydrated. Skin creams are rarely the answer here, but rather you’ll want to hydrate your skin from the inside out by consuming high quality, animal-based omega-3 fats in your diet.
Your best sources for omega-3s are animal-based fats like krill oil or fish oil. I also find it helpful to include a bit of gamma linoleic acid, typically in the form of primrose oil, as this works remarkably well for eczema. Products like “krill for women” are good for both sexes for this condition as they have both fatty acids.
Plant-based omega-3s like flax and hemp seed, although decent omega-3 sources in general, will not provide the clinical benefit you need to reduce inflammation and swelling in your skin.
Secondly, you’ll want to reduce your exposure to harsh soaps and drying out your skin with excessive bathing. Use a very mild soap when you cleanse your skin, especially in the winter to avoid stripping your skin of moisture.
Taking care of your gut = Taking care of your skin – Many don’t realize this, but the health and quality of your skin is strongly linked to the health of your gut. I recommend taking a high-quality probiotic to ensure optimal digestive health. Fermented foods can be used as well, but are neither as common nor as easy to use.
Diet and skin quality – Food allergies play an enormous role in eczema. In my experience, the most common offending agent is wheat, or more specifically, gluten. Avoiding wheat and other gluten-containing grains is therefore, a wise first step.

If you were to visit my clinic outside of Chicago as a new patient, one of the first steps we would advise would be to go on a gluten-free diet for a number of weeks and carefully observe any health improvements. This is an enormously common problem and many of our patients are surprised to find how much improvement they actually achieve from this step.
Avoiding grains will also reduce the amount of sugar in your system, which will normalize your insulin levels and reduce any and all inflammatory conditions you may have, including inflammation in your skin.
Other common allergens include milk and eggs. I recommend you do an elimination trial with these foods as well. You should see some improvement in about a week, sometimes less, after eliminating them from your diet if either of them is causing you trouble.
Basking in the sun – Vitamin D in the form of sun exposure is your best friend when dealing with either of these skin conditions, but it’s especially helpful for psoriasis.

I produced a one-hour lecture that explains the health benefits of this long under-appreciated vitamin, so if you haven’t seen it already, I strongly recommend you take the time to watch this free video now.
This video is a must to understand Vitamin D
https://youtu.be/vS9acVgQjZY
Ideally, you’ll want to get your vitamin D from appropriate sunshine exposure because UVB radiation on your skin will not only metabolize vitamin D but will also help restore ideal skin function. High amounts of UVB exposure directly on affected skin – but not so much to cause sunburn! – will greatly improve the quality of your skin.
However, if you can’t get sufficient amounts of sun during the winter months, a high-quality safe tanning bed can suffice. A safe tanning bed will provide the optimized forms of UVA and UVB wavelengths, without dangerous magnetic skin balance.
Why Conventional Treatments Fail
You don’t have to use expensive, dangerous medicines to treat eczema or psoriasis!
Steroid creams especially, are clearly something you’ll want to avoid, because although they work initially, you will tend to rapidly develop tolerance to them. These creams contain synthetic steroids, which are absorbed into your skin, and can wreak serious havoc with your adrenal system.
So please, avoid steroid creams and other potentially dangerous medications for these skin conditions and use these natural methods instead. You’ll find they work almost all the time, especially if you diligently apply them.
Western Medicine believe
from: https://en.wikipedia.org/wiki/Psoriasis
Psoriasis has a potential to be long-lasting autoimmune disease characterized by patches of crusty skin. These skin patches are typically red, itchy, and scaly. They may vary in severity from small and localized to complete body coverage. Injury to the skin can trigger psoriatic skin changes at that spot, which is known as Koebner phenomenon.
There are five main types of psoriasis: plaque, guttate, inverse, pustular, and erythrodermic. Plaque psoriasis, also known as psoriasis vulgaris, makes up about 90% of cases. It typically presents with red patches with white scales on top. Areas of the body most commonly affected are the back of the forearms, shins, around the navel, and the scalp. Guttate psoriasis has drop-shaped lesions. Pustular psoriasis presents with small non-infectious pus-filled blisters. Inverse psoriasis forms red patches in skin folds. Erythrodermic psoriasis occurs when the rash becomes very widespread, and can develop from any of the other types. Fingernails and toenails are affected in most people at some point in time. This may include pits in the nails or changes in nail color.
Psoriasis is generally thought to be a genetic disease which is triggered by environmental factors. In twin studies, identical twins are three times more likely to both be affected compared to non-identical twins; this suggests that perhaps genetic factors predispose to psoriasis. Symptoms often worsen during winter and with certain medications such as beta blockers or NSAIDs. Infections and psychological stress may also play a role. Psoriasis is not contagious. The underlying mechanism involves the immune system reacting to skin cells. Diagnosis is typically based on the signs and symptoms.
Various treatments can help control the symptoms. These treatments may include vitamin D3 cream, ultraviolet light. About 75% of cases can be managed with creams alone. It affects 2–4% of the population. Men and women are affected with equal frequency.
Underneath the Skin
The Genetic Link
If you have psoriasis, it’s possible that someone in your family may have had it too. That’s because there appears to be a genetic link for psoriasis.
One out of 3 people with psoriasis reports having a relative with the disease. And researchers say that up to 10% of the general population may inherit one or more genes that predispose them to psoriasis, though only 2% to 3% of people with the gene actually develop the disease.
Environmental Triggers
While psoriasis is most often linked with external allergic triggers, eczema is often caused by food allergies. The most common allergens include wheat, nuts, seafood, eggs and some fruits, such as strawberries.
Psoriasis is often associated with food intolerances and multiple chemical sensitivities. If you have been regularly reading my articles, this will likely ring a bell, since food intolerances and multiple chemical sensitivities are often the result of dysbiosis or an imbalance of intestinal flora that causes yeast overgrowth. This is sometimes accompanied with widespread systemic effects.
Another major cause of psoriasis is SAD — the dreaded Standard American Diet — which is rich in sugar and processed and refined foods. This sugar-filled diet eventually begins to wreak havoc with many aspects of our health.
Science suggests eczema and psoriasis may be autoimmune disorders, which in allopathic medicine tends to be a “cop-out” diagnosis. Integrative medicine argues that our immune system does not attack a healthy body. However, the immune system will go into overdrive when the body becomes toxic. An example of this is the simple case of aspartame, the poisonous artificial sweetener. Most “diet” products contain aspartame, a substance that people take in hopes of losing weight or use as a “healthier” substitute for sweetened products. These people often end up with itchy rashes that can be indistinguishable from eczema.
A naturopathic doctor would say that in an attempt to eliminate aspartame, its metabolites are excreted to the skin surface where it causes irritation.
The Key Role of the Immune System
Your immune system is meant to protect you when an “intruder,” like a cold virus, enters your body. But sometimes the immune system mistakes your body’s healthy cells for intruders and attacks them. While the exact cause of psoriasis isn’t fully understood, scientists believe psoriasis is the result of several factors, including the immune system.
When you have psoriasis, your immune system is overactive. This creates inflammation inside the body, which is a cause of the symptoms you see on the skin. More healthy cells are produced than normal. Those excess cells get pushed to the surface of your skin too quickly. Normally, it takes about a month for your skin cells to cycle through your body. With psoriasis, it takes days.
Your body simply can’t shed skin cells that quickly, so the cells build up on the surface of your skin. The thick, red patches you see on your skin (called plaques) are actually a buildup of excess skin cells.
Psoriasis and Comorbidities
When a person has two or more diseases at one time, these are called “comorbidities.”
Comorbidities associated with psoriasis include other immune conditions such as psoriatic arthritis and Crohn’s disease.
It’s important to keep your doctor informed about any symptoms you may be having so the two of you can decide how to possibly avoid or manage comorbidities.
Other Comorbidities
Psoriasis has been linked to other health conditions. Psoriasis is not thought to cause these conditions or vice versa. Patients with psoriasis have a greater likelihood of being diagnosed with the following conditions:
-
Psoriatic Arthritis
-
Type 2 diabetes
-
Cardiovascular disease
-
High blood pressure
-
Crohn’s Disease
-
High cholesterol
-
Depression
-
Ulcerative colitis
Here are some herbs/natural remedies that may help with your psoriasis or psoriatic arthritis.
from: https://www.psoriasis.org/treating-psoriasis/complementary-and-alternative/herbal-remedies
Aloe Vera
Gel from the aloe plant can be applied to the skin up to three times a day. Some research shows it can help reduce redness and scaling associated with psoriasis. Look for creams containing 0.5% aloe. No benefit has been shown from taking aloe in tablet form and it can be dangerous.
Apple Cider Vinegar
Used by ancient cultures as a disinfectant, apple cider vinegar may help relieve scalp itch from psoriasis. You can buy a bottle of organic apple cider vinegar at the grocery store and apply it to your scalp several times a week. Some people report diluting vinegar with water on a 1-to-1 ratio helps prevent a burning sensation. Others say they need to rinse the skin once the solution has dried to prevent irritation. Skip this cheap remedy if your scalp skin is cracked or bleeding. If you have open wounds, vinegar will only irritate your skin and cause a burning sensation. If it works for you, you should see results within a few weeks.
Capsaicin
Capsaicin is the ingredient in chili peppers that make them hot. Added to creams and ointments, capsaicin blocks nerve endings that transmit pain. Researchers from the University Medical Center Freiburg, in Freiburg, Germany, found OTC creams containing capsaicin may help reduce the pain, inflammation, redness and scaling associated with psoriasis. However, more research is needed to assess its long-term benefits and safety. Some people may feel a burning sensation where capsaicin ointment is applied.
Dead Sea Salts
Adding Dead Sea salts or Epsom salts to your warm (not hot) bath water and soaking in the tub for about 15 minutes may help remove scales and ease itching. Be sure to apply moisturizer to your skin as soon as you get out of the tub.
Oats
Oats are considered one of nature’s best skin soothers. There is no scientific evidence to support the use of oats to relieve psoriasis symptoms. But many individuals with psoriasis report applying an oat paste or taking a bath in oats relieves their itchy skin and reduces redness.
Tea tree oil
Tea tree oil is from the leaves of a plant that is native to Australia. Tea tree oil is believed to have antiseptic qualities and can be applied to the skin. Some people find using shampoos with tea tree oil helps relieve their scalp psoriasis.
Turmeric
This herb is being frequently studied for its powerful anti-inflammatory and antioxidant properties. Curcumin, the active ingredient in turmeric also has the ability to alter gene expression. A 2012 review by the International Union of Biochemistry and Molecular biology highlights turmeric’s ability to alter TNF cytokine expression. This is the likely reason some patients find it helpful in minimizing psoriasis and psoriatic arthritis flares. You can take turmeric concentrated in pill or supplement form or if you like curries, adding it liberally to your food. The FDA considers 1.5 to 3.0 grams of turmeric per day to be safe. However, we suggest that you consult with a naturopathic practitioner for help in determining the correct dosage for you.
Mahonia Aquifolium (Oregon Grape)
Mahonia is a powerful antimicrobial herb that plays a role in immune response. Studies show that applying a cream containing 10% mahonia is effective in treating mild to moderate psoriasis. Because it is in the alkaloid family, mahonia should only be used topical unless under physician supervision.
What therapies does Dr. Weil recommend for psoriasis?
from: http://www.drweil.com/drw/u/ART03161/Psoriasis.html
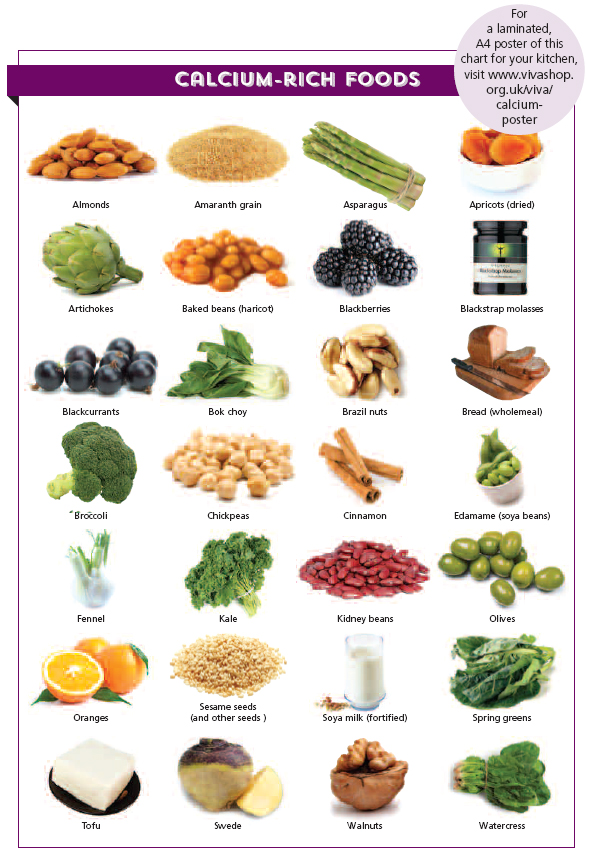
- Dietary changes: Follow an anti-inflammatory diet, making sure to get plenty of fresh fruits and vegetables, particularly those rich in carotenoids (mangoes, corn, sweet potatoes, carrots, and squash, as well as leafy greens and tomatoes).
- Exercise: Regular physical activity may help.
- Mind/body: Learn breathing exercises, yoga or visualization, or keep a journal recording your experiences, feelings, and skin symptoms. Since the skin is very responsive to hypnotic suggestion, hypnotherapy is definitely worth exploring.
- Traditional Chinese medicine: A TCM practitioner may recommend herbal preparations or acupuncture to help alleviate the condition.
- Supplements: Take supplemental omega-3 fatty acids (1-2 grams a day) and of evening primrose oil (500 mg twice a day), a natural source of GLA (gamma-linolenic acid), a fatty acid that promotes healthy growth of skin, hair and nails. Take extract of milk thistle (Silybum marianum), two capsules twice a day for at least three months.
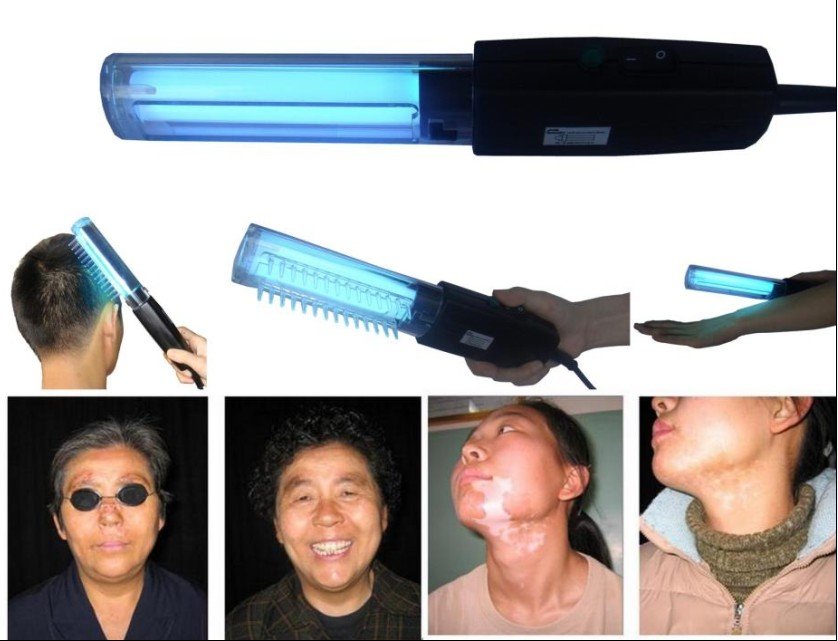
Phototherapy
from: https://www.psoriasis.org/about-psoriasis/treatments/phototherapy
Phototherapy or light therapy, involves exposing the skin to ultraviolet light on a regular basis and under medical supervision. Treatments are done in a doctor’s office or psoriasis clinic or at home with phototherapy unit. The key to success with light therapy is consistency.
National Psoriasis Foundation does not support the use of indoor tanning beds as a substitute for phototherapy performed with a prescription and under a doctor’s supervision. Indoor tanning raises the risk of melanoma by 59 percent, according to the American Academy of Dermatology and the World Health Organization, and does not provide the type of light that most effectively treats psoriasis.
Ultraviolet light B (UVB)
UVB phototherapy
Present in natural sunlight, ultraviolet B (UVB) is an effective treatment for psoriasis. UVB penetrates the skin and slows the growth of affected skin cells. Treatment involves exposing the skin to an artificial UVB light source for a set length of time on a regular schedule. This treatment is administered in a medical setting or at home.
There are two types of UVB treatment, broad band and narrow band. The major difference between them is that narrow band UVB light bulbs release a smaller range of ultraviolet light. Narrow-band UVB is similar to broad-band UVB in many ways. Several studies indicate that narrow-band UVB clears psoriasis faster and produces longer remissions than broad-band UVB. It also may be effective with fewer treatments per week than broad-band UVB.
During UVB treatment, your psoriasis may worsen temporarily before improving. The skin may redden and itch from exposure to the UVB light. To avoid further irritation, the amount of UVB administered may need to be reduced. Occasionally, temporary flares occur with low-level doses of UVB. These reactions tend to resolve with continued treatment.
UVB can be combined with other topical and/or systemic agents to enhance efficacy, but some of these may increase photosensitivity and burning, or shorten remission. Combining UVB with systemic therapies may increase efficacy dramatically and allow for lower doses of the systemic medication to be used.
Home UVB phototherapy
Treating psoriasis with a UVB light unit at home is an economical and convenient choice for many people. Like phototherapy in a clinic, it requires a consistent treatment schedule. Individuals are treated initially at a medical facility and then begin using a light unit at home.
It is critical when doing phototherapy at home to follow a doctor’s instructions and continue with regular check-ups. Home phototherapy is a medical treatment that requires monitoring by a health care professional.
All phototherapy treatments, including purchase of equipment for home use, require a prescription. Some insurance companies will cover the cost of home UVB equipment. Vendors of home phototherapy equipment often will assist you in working with your insurance company to purchase a unit.
Sunlight
Although both UVB and ultraviolet light A (UVA) are found in sunlight, UVB works best for psoriasis. UVB from the sun works the same way as UVB in phototherapy treatments.
Short, multiple exposures to sunlight are recommended. Start with five to 10 minutes of noontime sun daily. Gradually increase exposure time by 30 seconds if the skin tolerates it. To get the most from the sun, all affected areas should receive equal and adequate exposure. Remember to wear sunscreen on areas of your skin unaffected by psoriasis.
Avoid overexposure and sunburn. It can take several weeks to see improvement. Have your doctor check you regularly for sun damage.
Some topical medications can increase the risk of sunburn. These include tazarotene, coal tar, Elidel (pimecrolimus) and Protopic (tacrolimus). Individuals using these products should talk with a doctor before going in the sun.
People who are using PUVA or other forms of light therapy should limit or avoid exposure to natural sunlight unless directed by a doctor.
Psoralen + UVA (PUVA)
Like UVB, ultraviolet light A (UVA) is present in sunlight. Unlike UVB, UVA is relatively ineffective unless used with a light-sensitizing medication psoralen, which is administered topically or orally. This process, called PUVA, slows down excessive skin cell growth and can clear psoriasis symptoms for varying periods of time. Stable plaque psoriasis, guttate psoriasis, and psoriasis of the palms and soles are most responsive to PUVA treatment.
The most common short-term side effects of PUVA are nausea, itching and redness of the skin. Drinking milk or ginger ale, taking ginger supplements or eating while taking oral psoralen may prevent nausea. Antihistamines, baths with colloidal oatmeal products or application of topical products with capsaicin may help relieve itching. Swelling of the legs from standing during PUVA treatment may be relieved by wearing support hose.
Laser Treatments
Excimer laser
The excimer laser—recently approved by the Food and Drug Administration (FDA) for treating chronic, localized psoriasis plaques—emits a high-intensity beam of ultraviolet light B (UVB).
The excimer laser can target select areas of the skin affected by mild to moderate psoriasis, and research indicates it is a particularly effective treatment for scalp psoriasis. Researchers at the University of Utah, for example, reported in The Journal of Drugs in Dermatology that in a small series of patients, laser treatment, combined with a topical steroid, cleared scalp psoriasis that resisted other treatment.
Individual response to the treatment varies. It can take an average of four to 10 sessions to see results, depending on the particular case of psoriasis. It is recommended that patients receive two treatments per week, with a minimum of 48 hours between treatments.
DIET AND PSORIASIS
Generally speaking, there are four main approaches to diet:
from: https://www.psoriasis.org/about-psoriasis/treatments/alternative/diet-supplements
Weight-loss
A 2014 study published in the Journal of the American Academy of Dermatology linked obesity to an increased risk for psoriatic disease. Researchers found that a higher body mass index (BMI) is associated with an elevated risk for developing psoriasis and psoriatic arthritis, as well as an increase in the severity of the disease.
Dr. Wilson Liao, the study’s co-author, said that obesity may provide the nudge that triggers psoriasis in people who are already predisposed to it. The researchers also found that in overweight individuals, losing weight may improve the effectiveness of treatments. Fat cells secrete cytokines, which are proteins that can trigger inflammation, explained Liao. “So if you lose weight, you may be reducing fuel for the fire.”
A study from the same year in the British Journal of Dermatology also identified an association between weight loss and a reduction in psoriasis severity. This study focused on a “dietary intervention” combined with systemic treatment, including exercise, over the course of 20 weeks.
“There was a clear correlation between the amount of weight loss and the improvement of psoriasis,” said Dr. Luigi Naldi, the BJD study’s lead author. “Patients who lost more weight experienced a larger improvement in psoriasis,” he said. Even a small amount of weight loss can have a big impact on disease severity, he added.
The long-term impact of a dietetic intervention on psoriasis remains to be explored. But the results of this study emphasize the importance of weight loss as part of an overall treatment for psoriasis and its comorbid conditions in overweight patients with psoriasis.
Other incentives
In addition to the improvement in psoriasis severity indicated by these results, there are numerous other incentives for obese patients with psoriasis to lose weight. Psoriasis, especially if severe, is associated with an increased risk of cardiovascular morbidity and mortality. Weight loss improves cardiovascular risk factors (e.g. arterial hypertension, diabetes and high cholesterol). Also, obesity may diminish the therapeutic effect of certain medications.
“We know that fat is an inflammatory tissue, so maintaining a healthy weight—and reducing overall body fat—may result in a reduction in systemic inflammation,” said Dr. Nehal Mehta, a cardiologist at the National Institutes of Health who studies metabolic disorders and systemic inflammation. “We think that this may, in turn, help with improvement in symptoms of psoriasis and psoriatic arthritis.”
“We all have to eat during the day,” said Dr. Liao. “If there’s a way to turn that requirement into a benefit for our health and for psoriasis, then why not?”
Let’s get started
To help identify what is a healthy weight for you, calculate your body mass index (BMI.) You can use this calculator from the Centers for Disease Control and Prevention.
To lose weight, you must burn more calories than you consume. One pound equals 3,500 calories. If you cut 500 a day from your diet, you’ll lose a pound a week. People who lose weight slowly, about 1 to 2 pounds per week, are more successful at keeping the weight off. You’ll also burn additional calories if you increase your physical activity.
You weight-loss plan should do all of the following:
- Emphasize fruits, vegetables, whole grains, and fat-free or low-fat dairy products.
- Include lean meats, poultry, fish, beans, eggs, and nuts.
- Contain foods low in saturated fats, avoid trans fats, and limit cholesterol and salt (sodium).
- Avoid refined sugars and processed foods
Some tips to help you lose weight:
- Keep a food diary. Writing down everything you eat is critical! Noting how you feel when you eat will help you identify emotional triggers that may cause you to overeat. Emotional eaters tend to overeat.
- Eat when you’re truly hungry rather than when you’re tired, anxious or stressed.
- Eat slowly. If you eat too fast, you eat more than you need to satisfy your hunger. Your brain needs time to catch up with your stomach.
- Plan your meals ahead of time so you make healthy choices. When dining out, check the menu online and decide what you will order before you sit down. Ask for dressings on the side. Opt for foods that are baked, broiled or steamed versus fried or swimming in creamy sauces. Avoid chips and bread baskets—they add unnecessary calories.
- Stay hydrated. People often mistake thirst for hunger.
- Eat breakfast. If you skip this meal, you’ll be starving by lunchtime. You’ll have more difficulty making healthy choices throughout the day.
- Find resources to help you keep track of your food choices and nutritional values, and that can offer additional support when you need it. Try CalorieKing.com and MyFitnessPal.com, which offer a searchable database of foods with nutritional values.
- Before you get started, consult your doctor!
Heart-healthy
Psoriasis is an inflammatory disease, the same as heart disease. Reducing inflammation and improving heart health are important for people with psoriasis. Here are some recommendations for heart-healthy eating:
- Eat fish at least twice a week. Cold-water fish (such as albacore tuna, mackerel, salmon, herring, and lake trout) contain omega-3 fatty acids that can help lower your risk of coronary artery disease.
- Choose lean meats and poultry without skin. Prepare them without adding saturated fat or trans fat. Baking and broiling are heart-healthy ways to prepare lean meats and poultry.
- Use fat-free, 1 percent fat, and low-fat dairy products.
- Limit foods containing partially hydrogenated vegetable oils. They contain trans-fat.
- Shoot for less than 1,500 milligrams of sodium per day. Read food labels to see how much sodium you’re consuming.
- Limit alcohol. If you have severe psoriasis, you may benefit from eliminating alcohol entirely. If you are going to have an occasional drink, the recommendations are: women no more than one drink per day, men no more than two.
- Keep an eye on your portion sizes. Consider weighing and measuring your food until you get used to appropriate sizes.
- Limit the amount of processed and fast food you eat.
Anti-inflammatory
Psoriasis is an inflammatory disease. Many individuals have benefitted from following an anti-inflammatory diet to help reduce their symptoms.
“The response to any medical intervention will vary based on individual circumstances, compliance to the recommendations, and genetics,” said Dr. Andrew Weil, who directs the Center for Integrative Medicine at the University of Arizona and is the author of numerous best-selling books on diet and health. “However, in my experience, most people respond well to dietary and lifestyle modifications aimed at controlling chronic inflammation.”
Foods to avoid because they have been shown to cause or increase inflammation:
- Fatty red meats
- Dairy products
- Processed foods
- Refined sugars
- Nightshade vegetables, including potatoes, tomatoes, and peppers
Foods to include in your diet that have been shown to reduce inflammation:
- Cold-water fish (see the Heart-Healthy diet above).
- Flaxseeds, olive oil, pumpkin seeds, and walnuts. These are plant sources of omega-3 fatty acids.
- Colorful fresh fruits and vegetables. Choose foods from the colors of the rainbow.
Nutritious examples are:
- Carrots
- Squash and sweet potatoes
- Spinach
- Kale and broccoli
- Blueberries
- Mangoes
- Strawberries and figs
Gluten-free
Many people with psoriasis and/or psoriatic arthritis who are looking for treatments that don’t involve drugs are interested in gluten-free diets. They wonder if these diets will improve their condition.
Many studies have evaluated the benefits of a gluten-free diet for psoriasis. The link between psoriasis and gluten (a complex protein found in wheat, barley and rye and in many processed foods, from lunch meats to salad dressings) is not well understood, but new research estimates that up to 25 percent of people who have psoriasis may also be sensitive to gluten. Celiac disease is caused by an intolerance to gluten. A gluten-free diet is the only known treatment for celiac disease.
A number of studies suggest that psoriasis and celiac disease share common genetic and inflammatory pathways. Research further suggests that having psoriasis about doubles your chance of being diagnosed with celiac disease.
There is no published evidence that going on a gluten-free diet can improve psoriasis in people who do not have celiac disease – but there is anecdotal evidence from people who have tried the gluten-free diet and swear by it.
If you suspect you may have celiac disease or cannot tolerate gluten, you may be tempted to eliminate gluten from your diet on your own. But experts advise that you first schedule a blood test to check for the allergy. Talk to your doctor and/or a registered dietitian on how to start a gluten-free regimen.
If you eliminate more than one food at a time, for example, it can be hard to know which food or foods were actually the problem. It could take up to 90 days for any inflammation to subside. A dietician can help you make a list of gluten-free foods to make sure you get the nutrients your body needs.
It is also possible that gluten isn’t contributing to your symptoms, but that another food such as dairy, sugar, corn or soy might be.
The challenges of a gluten-free diet
Following a gluten-free diet requires you to become educated on all the hidden sources of gluten, as well as educating everyone you live with. To avoid all gluten, you must read labels carefully. You must avoid not only wheat but its derivatives: durum, graham, kamut, semolina and spelt. The same goes for barley derivatives: malt flavoring and malt vinegar, as well as rye, MSG and soy sauce.
Read labels regularly. Manufacturers change ingredients without notice.
Just because a food is labeled wheat-free doesn’t mean it’s gluten-free. And just because a food is labeled gluten-free doesn’t mean it’s calorie-free. Some manufacturers add sugar, saturated fats and preservatives to their gluten-free offerings to make them taste better, and that adds calories.
You can still eat a balanced diet when you’re trying to avoid gluten. Gluten-free diets allow you to eat fresh fruits and vegetables. Beef, chicken, fish, lamb, pork and dairy products are also naturally gluten-free. (But watch for additives.)
For someone with psoriasis who does not also have celiac disease and is not allergic to gluten, giving up gluten may not be such a good idea. Following a gluten-free diet is a major commitment. It can be difficult to maintain a balanced diet while eliminating the many foods that contain gluten. It’s not a step you should take unnecessarily.
The bottom line on gluten
Eliminating gluten from your diet may help reduce your psoriasis symptoms as well as eliminate digestive woes, but it’s only likely to help if gluten is a problem food for you in the first place.
Vitamins and Supplements
Studies have not shown a direct link between vitamins and dietary supplements and psoriatic disease. Yet many people with psoriasis and psoriatic arthritis find that including vitamins and supplements in their diet helps clear their skin and may ease joint pain.
Dietary supplements can be extracts or concentrates, and they can occur in many forms, such as tablets, capsules, softgels, gelcaps, liquids or powders.
Omega-3 fatty acids have been shown to decrease inflammation, and psoriasis is a disease of inflammation. Omega-3 fatty acids also seem to have a positive impact on the body’s immune system.
There are three types of omega-3 fatty acids:
- Alpha-linolenic acid
- Eicosapentaenoic acid (EPA)
- Docosahexaenoic acid (DHA)
Alpha-linolenic acid is found in some vegetable oils, nuts, seeds and soy foods. EPA and DHA are found in fatty fish and algae. Fish oil also is available in capsule form as a supplement. Some individuals with psoriasis show a deficiency of omega-3 fatty acids and elevations of omega-6 fatty acids, which tend to increase inflammation.
The research on whether omega-3 fatty acid supplements can help reduce the severity of psoriasis is mixed. More long-term clinical controlled studies are needed.
Fish oil can thin your blood, so check with your doctor before you start taking it and especially if you are taking Coumadin (warfarin) or other blood thinners.
Vitamin D topical ointments have been around and used to treat psoriasis for some time. Vitamin D is the main active ingredient in two prescription medications – Vectical and Dovonex – that are applied to the skin. Psoriasis increases the growth of the skin’s cells. Vitamin D can change the way cells grow and may slow their growth.
Research on whether vitamin D can help alleviate psoriasis symptoms is small and limited. A report in the May 2011Science Translational Medicine journal found that vitamin D helps counteract the body’s response to inflammation associated psoriasis.
Too much vitamin D can be dangerous. Dr. Wilson Liao, co-author of the 2014 study on diet and psoriasis that appeared in the Journal of the American Academy of Dermatology, warned that vitamin D can also cause serious side effects by raising the calcium level in the blood. “Sometimes that can lead to things like kidney stones and maybe even gout,” he said.
Before you add vitamin D to your psoriasis regimen, talk with your doctor. The safest source of vitamin D is food:
- Cod liver oil
- Salmon (sockeye)
- Mackerel
- Tuna fish canned in water
- Milk, non-fat, reduced fat, and whole, vitamin D-fortified
- Orange juice fortified with vitamin D
- Yogurt fortified with 20 percent of the daily value of vitamin D
- Eggs, vitamin D is found in the egg yolk
- Swiss cheese
- Fortified cereals
You also can get vitamin D from 10 minutes of midday exposure to the sun. (Prolonged sun exposure has been linked to aging skin and skin cancer and is not recommended!)
A simple blood test can tell you whether you’re deficient in vitamin D.
Glucosamine and chondroitin are over-the-counter dietary supplements that can be taken individually or together. They occur naturally in and around the cells of cartilage in the body.
- Glucosamine may help in cartilage formation and repair and possibly inhibit inflammation.
- Chondroitin may promote cartilage elasticity and inhibit the breakdown of cartilage.
A growing body of research shows that these supplements may slow the progression and reduce the pain of osteoarthritis, a degenerative disease characterized by cartilage deterioration of the joints. However, psoriatic arthritis and osteoarthritis are different forms of arthritis and have different symptoms. No studies have found that glucosamine and/or chondroitin supplements effectively reduce symptoms of psoriatic arthritis.
Glucosamine contains substances extracted from animal tissue including shrimp, lobster shells and shark cartilage. People who are allergic to shellfish should avoid glucosamine. Also, children and women who are pregnant or plan to become pregnant should not take these supplements. Glucosamine has been shown to increase blood sugar levels in some people with diabetes. If you have diabetes, talk with your doctor before taking glucosamine supplements.
Methylsulfonylmethane (MSM) is an organic sulfur-containing compound found in plants, fruits, and vegetables. However, it is destroyed when food is processed. The body needs sulfur to maintain healthy connective tissue.
You can buy MSM as a dietary supplement. However, there is little scientific evidence that it relieves joint pain or has anti-inflammatory benefits. One 2006 study by researchers at the Southwest College Research Institute in Tempe, Ariz., found that MSM improved symptoms of pain and physical function in patients with knee osteoarthritis without major adverse events. More research is needed.
https://youtu.be/-zckble4p-w
Natural Plaque Psoriasis Treatment & Skin Care Serum With 100% Pure Argan Oil
- Helps Alleviate Dry, Scaly Skin: Infused with 100% pure, naturally soothing Argan Oil, tea tree oil & Vitamin E, our treatment gently yet effectively sloughs away psoriasis plaques & relieves itching, redness& inflammation. Enjoy relief and renewed confidence! aques. Perfect for nighttime use.
- All Natural Formula: Our herbal therapy is free of steroids, coal tar, salicylic acid & other potentially toxic ingredients. It’s hypoallergenic and suitable for sensitive skin, with no harsh preservatives or artificial dyes. Lightly fragranced with essential oils.
- Fast Acting: No waiting for months to see results-many customers report seeing dramatic psoriasisimprovement in just a few days! Our non-drying serum can be used on a long-term basis and will continue to work with regular application.
- Non-Greasy: Unlike topical creams that are greasy and cakey, our concentrated formula is quickly & invisibly absorbed into your skin. While the active ingredients go to work, your skin is soft and moisturized. Use any time of day.
Honeyskin Organics Aloe Vera + Manuka Honey Face and Body Cream for Rosacea, Eczema, Psoriasis, Rashes, Itchiness, Redness with raw Superfoods
- Our SUPERIOR, Organic, Natural and Nutrient Rich Anti-oxidant Cream uses Aloe Vera as the first ingredient to soothe, Powerful medical grade Manuka Honey for healing and MSM for inflammation, as well as Cocoa Butter, Coconut Oil, Shea Butter, Hempseed Oil, Vitains A, C and E, Trace Minerals from Blue-Green Algae and botanicals the skin CRAVES, all working together to give you the best SKIN CARE possible.
- Non-Greasy, Absorbs Fully for FAST relief, helps to effectively treat Eczema, Rashes, Psoriasis, Rosacea, Shingles, Redness and Itching. The cream penetrates fully to work INSIDE, not on top.
- BEAUTIFUL SKIN IS HEALTHY SKIN – Need an effective anti-wrinkle cream? Our cream contains every Vitamin, Mineral, Trace Mineral and Amino Acid your skin needs to FIX itself! Collagen stimulators, anti-inflammatories an botanicals work at HYDRATING and RESTORING the skin, PH balanced perfectly at 5.5 for face and eyes as well.
Certified Organic PSORIASIS-ECZEMA Soap – by Vi-Tae
- Clearer Skin & Itch Relief: Dry, itchy, and sensitive skin can lead to great discomfort. But packed with Calendula Petals, Grape Seed, and Evening Primrose Oil, our Psoriasis/Eczema Soap can naturally relieve symptoms and inflammation, giving you clear, nourished skin!
- Hydrate Your Skin: If you suffer from Psoriasis or Eczema, you know that most soaps will irritate your condition. But not ours! Anti-inflammatory ingredients like Coconut, Jojoba, and Safflower Oil make this soap great for all skin types by preventing dry, irritated skin.
The Fay Farm’s Organic Healing Hemp Lotion
- Natural relief for Eczema, Psoriasis and other auto-immune skin disorders.
- Fast absorbing, light
- Also great for Dermatitis, burns, cracked heals, and cuticles.